 Cleft lip (cheiloschisis) and cleft palate (palatoschisis) are among the most common birth defects affecting children in North America. The incomplete formation of the upper lip (cleft lip) or roof of the mouth (cleft palate) can occur individually, or both defects may occur together. The conditions can vary in severity and may involve one or both sides of the face.
Cleft lip (cheiloschisis) and cleft palate (palatoschisis) are among the most common birth defects affecting children in North America. The incomplete formation of the upper lip (cleft lip) or roof of the mouth (cleft palate) can occur individually, or both defects may occur together. The conditions can vary in severity and may involve one or both sides of the face.
A cleft, or separation of the upper lip and/or the roof of the mouth, occurs very early in the development of your unborn child. During fetal development, certain components of the upper lip and roof of the mouth fail to form normally. Cleft lip and cleft palate repair is a type of plastic surgery to correct this abnormal development both to restore function and to restore a more normal appearance.
Most clefts can be repaired through specialized plastic surgery techniques, improving your child’s ability to eat, speak, hear and breathe, and to restore a more normal appearance and function.
A team of specialists can help
Early intervention by a team of specialists to evaluate your child is essential in cleft lip and/or cleft palate repair. The team can work together to define a course of treatment, including surgical repair of the cleft, speech rehabilitation and dental restoration. These specialists may include a:
- Plastic surgeon
- Pediatrician
- Pediatric dentist
- Otolaryngologist (ear, nose, and throat specialist)
- Auditory or hearing specialist
- Speech pathologist
- Genetic counselor
- Social worker
 Surgery to repair a cleft of any kind is a highly individualized procedure that’s intended to not only close the defect, but also to insure your child’s ability to function and grow normally.
Surgery to repair a cleft of any kind is a highly individualized procedure that’s intended to not only close the defect, but also to insure your child’s ability to function and grow normally.
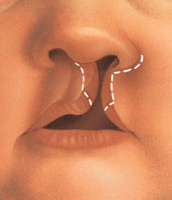
Cleft lip repair, also called cheiloplasty, includes reconstruction of a more normal appearance, namely:
- Closure of the cleft resulting in a scar located in the normal structures of the upper lip
- Formation of a cupid’s bow (the curve at the center of the upper lip)
- Considerations for adequate distance between the upper lip and nose
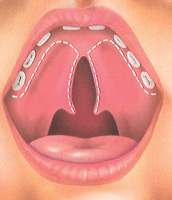
Because the palate creates the floor of the nasal cavity, considerations in repairing a cleft palate include:
- Allowing for normal growth, function and speech development
- Relation of the palate to the auditory canal and hearing
- Development of the teeth and jaw alignment
Where the cleft also affects the shape of the nose, additional procedures may be recommended to:
- Achieve symmetry between the nostrils
- Create adequate length of the columella (the tissue that separates the nostrils)
- Increase the angle of the nasal tip, to avoid a flattened nasal tip or one that pulls downward
When should my child have the surgery?
The timing of the cleft repairs depend on the individual circumstances of your child.
Cleft lip repairs are initially performed when a child is at least 10 weeks of age and 10 pounds in weight and has a hemoglobin (or blood count) of at least 10.
Cleft palate repairs are generally performed when a child is somewhat older, from 9 to 18 months of age.
Cleft repair may be delayed in order to treat other, more life-threatening problems that may be present such as a heart or lung disorder.
The success and safety of your child’s cleft procedure starts with a consultation with a plastic surgeon and depends very much on your complete candidness.
 Be prepared to discuss:
Be prepared to discuss:
- Your concerns and an evaluation of your child’s condition
- Options available for cleft lip and/or cleft palate repair
- Likely outcomes of surgery and the potential risks and complications associated with the procedure
- A recommended course of treatment
Be candid about your concerns for your child and your plastic surgeon’s ability to meet his or her special needs. The success of your child’s procedure, safety and overall satisfaction requires that you:
- Honestly share your concerns
- Fully disclose your child’s health history including current medications, vitamins, and herbal supplements
- Commit to precisely following all of your plastic surgeon’s instructions
 Prior to surgery, your plastic surgeon will discuss with you:
Prior to surgery, your plastic surgeon will discuss with you:
- Pre-surgical considerations, diagnostic testing and medications
- Day-of-surgery instructions and medications
- Specific information related to the use of anesthesia
- Postoperative care and follow-up
Your plastic surgeon will also discuss where your child’s procedure will be performed. Cleft repair is generally performed in a hospital setting.
Prior to surgery: In some cases, your child may be given an intraoral (inside the mouth) device, called an obturator, to wear prior to repair of the cleft lip which may assist in feeding and maintain the arch of the lip prior to repair.
Step 1 – Anesthesia
Medications are administered for your child’s comfort during the surgical procedures. The choices include intravenous sedation and general anesthesia. Your doctor will recommend the best choice for your child.
Step 2 – The incision
The goal of cleft lip surgery is to close the separation in the lip and to provide a more normal function, structure and appearance to the upper lip. Incisions are made on either side of the cleft to create flaps of tissue that are then drawn together and stitched to close the cleft.
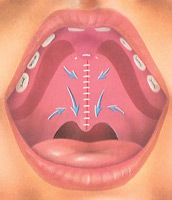
The repair of a cleft palate requires careful repositioning of tissue and muscles to close the cleft and rebuild the roof of the mouth. Incisions are made on either side of the cleft and specialized flap techniques are used to reposition muscle and the hard and soft components of the palate. The repair is then stitched closed, generally at the midline of the roof of the mouth, providing enough length of the palate to allow for normal feeding and speech development, and continued growth throughout life.
Step 3 – Closing the incisions
Cleft lip and palate incisions can be closed with removable or absorbable sutures.
A special note: It is important to understand that while a cleft may be surgically repaired in a single plastic surgery procedure, treating a child born with a cleft continues through adolescence and sometime even adulthood. As a child grows, secondary plastic surgery procedures to improve function and appearance may be required.
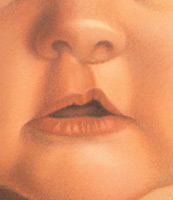
Step 4 – See the results
The resulting external scars of a cleft repair are generally positioned in the normal contours of the upper lip and nose. Over time, these will fade and your child’s ability to grow and function normally will continue to improve.
The decision to have cleft surgery is extremely personal and your plastic surgeon will explain the benefits, goals and potential risks or complications. Your plastic surgeon and/or staff will explain in detail the risks associated with surgery. You will be asked to sign consent forms to ensure that you fully understand the procedure, the alternatives and the most likely risks or potential complications.
Some of the risks include:
- Bleeding (hematoma)
- Infection
- Poor healing of incisions
- Irregular healing of scars including contracture (puckering or pulling together of tissues)
- Residual irregularities and asymmetries
- Anesthesia risks
- Allergies to tape, suture materials and glues, blood products, topical preparations or injected agents
- Damage to deeper structures — such as nerves, blood vessels, muscles, and lungs — can occur and may be temporary or permanent
- Possibility of revisional surgery
Be sure to ask questions: It’s natural to feel some anxiety, whether excitement for the anticipated outcomes for your child or preoperative stress. Please discuss these feelings with your plastic surgeon
After surgery, dressings or bandages may be placed on incisions outside your child’s mouth.
You will be given specific instructions that may include: How to care for the surgical site following surgery, medications to apply or take orally to aid healing and reduce the risk of infection, specific concerns to look for in the general health of your child, and when to follow-up with your plastic surgeon.
Your plastic surgeon or the attending staff will instruct you on feeding your child and as well as any restrictions or special activity instructions.
Don’t be surprised if you find that arm restraints have been placed on your child in recovery. They will prevent him or her from injuring the surgical site as it heals. Restraints may be removed several times as day, so long as your child is supervised and prevented from touching the surgical site or sucking a thumb.
Your child’s discomfort can be controlled with pain medication. If necessary, sutures will be removed following surgery. Healing will continue for several weeks as swelling resolves.
After surgery, diligent sun protection is essential to prevent the formation of irregular scars.
Results and outlook
The outcome of your child’s initial cleft lip and/or cleft palate repair will make a vast difference in his or her quality of life, ability to breathe, eat and speak. However, secondary procedures may be needed for functional reasons or to refine appearance. Even though the scars of a cleft lip repair are generally located within the normal contours of the face, they will always be visible.
Cost is always a consideration in surgery. A surgeon’s cost may vary based on his or her experience, the type of procedure used, as well as geographic location.
Cost may include:
- Surgeon’s fee
- Hospital or surgical facility costs
- Anesthesia fees
- Prescriptions for medication
- Post-surgery garments
- Medical tests
Your health insurance plans will likely cover cleft surgery because it is a reconstructive procedure. Be certain to check with your insurance carrier. Coverage varies among insurers including precertification requirements, coverage for secondary procedures and allied health care services such as speech therapy.
The American Society of Plastic Surgeons, in conjunction with the American Academy of Pediatrics, have co-authored a position statement regarding health care coverage for the reconstruction of abnormal appearance in children, including cleft repair. Ask your plastic surgeon for a copy of this document to file with your insurance claims.
Your satisfaction involves more than a fee
When choosing a plastic surgeon for your child’s cleft surgery, remember that the surgeon’s experience and your comfort with him or her are just as important as the final cost of the surgery.
- Auditory canal: A passage in the ear.
- Cheiloplasty: Cleft lip repair surgery.
- Cheiloschisis: The scientific term for a cleft lip.
- Cleft lip: The incomplete formation of the upper lip.
- Cleft palate: The incomplete formation of the roof of the mouth.
- Cleft: A separation of the upper lip and/or the roof of the mouth.
- Columella: Tissue that separates the nostrils.
- Contracture: A puckering or pulling together of tissues; a potential side effect of cleft surgery.
- General anesthesia: Drugs and/or gases used during an operation to relieve pain and alter consciousness.
- Hemoglobin: Blood count.
- Intraoral: Inside the mouth.
- Intravenous sedation: Sedatives administered by injection into a vein to help you relax.
- Obturator: An intraoral device your child may wear prior to repair of the cleft lip which may assist in feeding and maintain the arch of the lip prior to repair.
- Palatoschisis: The scientific term for a cleft palate.
Use this checklist as a guide during your consultation
- Are you certified by the American Board of Plastic Surgery?
- Are you a member of the American Society of Plastic Surgeons?
- Were you specially trained in the field of plastic surgery?
- Do you have hospital privileges to perform this procedure? If so, at which hospitals?
- Is the office-based surgical facility accredited by a nationally or state recognized accrediting agency, or is state licensed or Medicare-certified?
- How many procedures of this type have you performed?
- Is my child a good candidate for this procedure?
- What will be expected to get the best results?
- Where and how will you perform my child’s procedure?
- What shape, size, surface texturing, incision site and placement site are recommended for my child?
- How long of a recovery period can we expect, and what kind of help will my child need during my recovery?
- What are the risks and complications associated with this procedure?
- How are complications handled?
- What are my options if I am dissatisfied with the outcome of my child’s cleft surgery?
- Do you have before-and-after photos I can look at for each procedure and what are reasonable results?
Plastic surgery involves many choices. The first and most important is selecting a surgeon you can trust.
Choosing an ASPS Member Surgeon ensures that you have selected a physician who:
- Has completed at least five years of surgical training with a minimum of two years in plastic surgery.
- Is trained and experienced in all plastic surgery procedures, including breast, body, face and reconstruction.
- Operates only in accredited medical facilities
- Adheres to a strict code of ethics.
- Fulfills continuing medical education requirements, including standards and innovations in patient safety.
- Is board certified by The American Board of Plastic Surgery or in Canada by the Royal College of Physicians and Surgeons of Canada®.
ASPS Member Surgeons are your partners in cosmetic and reconstructive plastic surgery.
Look for the ASPS Member Surgeon logo.

 3510 N. Ridge Rd, Suite 100
3510 N. Ridge Rd, Suite 100