.jpg) Breast reconstruction is achieved through several plastic surgery techniques that attempt to restore a breast to near normal shape, appearance and size following mastectomy.
Breast reconstruction is achieved through several plastic surgery techniques that attempt to restore a breast to near normal shape, appearance and size following mastectomy.
Enhancing your appearance with breast reconstruction
Breast reconstruction is a physically and emotionally rewarding procedure for a woman who has lost a breast due to cancer or other condition.
The creation of a new breast can dramatically improve your self-image, self-confidence and quality of life. Although surgery can give you a relatively natural-looking breast, a reconstructed breast will never look or feel exactly the same as the breast that was removed.
Is it right for me?
Breast reconstruction is a highly individualized procedure. You should do it for yourself, not to fulfill someone else’s desires or to try to fit any sort of ideal image.
Breast reconstruction is a good option for you if:
- You are able to cope well with your diagnosis and treatment
- You do not have additional medical conditions or other illnesses that may impair healing
- You have a positive outlook and realistic goals for restoring your breast and body image
Breast reconstruction typically involves several procedures performed in multiple stages. It can:
- Begin at the same time as mastectomy, or
- Be delayed until you heal from mastectomy and recover from any additional cancer treatments
It’s important that you feel ready for the emotional adjustment involved in breast reconstruction. It may take some time to accept the results of breast reconstruction.
The success and safety of your breast reconstruction procedure depends very much on your complete candidness during your consultation. You’ll be asked a number of questions about your health, desires and lifestyle.
.jpg) Be prepared to discuss:
Be prepared to discuss:
- Why you want the surgery, your expectations and desired outcome
- Medical conditions, drug allergies and medical treatments
- Use of current medications, vitamins, herbal supplements, alcohol, tobacco and drugs
- Previous surgeries
- The options available in breast reconstruction surgery
- The likely outcomes of breast reconstruction and any risks or potential complications
- The course of treatment recommended by your plastic surgeon, including procedures to achieve breast symmetry
Your surgeon may also:
- Evaluate your general health status and any pre-existing health conditions or risk factors
- Examine your breasts, and take detailed measurements of their size and shape, skin quality, and placement of nipples and areolae
- Take photographs for your medical record
- Discuss your options and recommend a course of treatment
- Discuss likely outcomes of breast reconstruction and any risks or potential complications
.jpg) Prior to surgery, you may be asked to:
Prior to surgery, you may be asked to:
- Get lab testing or a medical evaluation
- Take certain medications or adjust your current medications
- Stop smoking well in advance of surgery
- Avoid taking aspirin, anti-inflammatory drugs and herbal supplements as they can increase bleeding
Special instructions you receive will cover:
- What to do on the day of surgery
- The use of anesthesia during your breast reconstruction
- Post-operative care and follow-up
- Breast implant registry documents (when necessary)
Your plastic surgeon will also discuss where your procedure will be performed. Breast reconstruction surgery may be performed in an accredited office-based surgical center, outpatient/ambulatory surgical center, or a hospital.
You’ll need help
If your breast reconstruction is performed on an outpatient basis, be sure to arrange for someone to drive you to and from surgery and to stay with you for at least the first night following surgery.
Breast reconstruction is achieved through several plastic surgery techniques that attempt to restore a breast to near normal shape, appearance and size following mastectomy.
 Although breast reconstruction can rebuild your breast, the results are highly variable:
Although breast reconstruction can rebuild your breast, the results are highly variable:
- A reconstructed breast will not have the same sensation and feel as the breast it replaces.
- Visible incision lines will always be present on the breast, whether from reconstruction or mastectomy.
- Certain surgical techniques will leave incision lines at the donor site, commonly located in less exposed areas of the body such as the back, abdomen or buttocks.
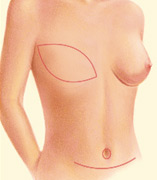
A note about symmetry: If only one breast is affected, it alone may be reconstructed. In addition, a breast lift, breast reduction or breast augmentation may be recommended for the opposite breast to improve symmetry of the size and position of both breasts.
The decision to have breast reconstruction surgery is extremely personal. You’ll have to decide if the benefits will achieve your goals and if the risks and potential complications are acceptable.
Your plastic surgeon and/or staff will explain in detail the risks associated with surgery. You will be asked to sign consent forms to ensure that you fully understand the procedures you will undergo and any risks or potential complications.
The possible risks of breast reconstruction include, but are not limited to, bleeding, infection, poor healing of incisions, and anesthesia risks. You should also know that:
- Flap surgery includes the risk of partial or complete loss of the flap and a loss of sensation at both the donor and reconstruction site.
- The use of implants carries the risk of breast firmness (capsular contracture) and implant rupture.
Breast implants do not impair breast health. Careful review of scientific research conducted by independent groups such as the Institute of Medicine has found no proven link between breast implants and autoimmune or other systemic diseases. Visit www.breastimplantsafety.org for current information.
Where will my surgery be performed?
Surgery for your breast reconstruction is most often performed in a hospital setting, possibly including a short hospital stay, and your doctor will likely use general anesthesia.
Some follow-up procedures may be performed on an outpatient basis, and local anesthesia with sedation may be used.
These decisions will be based on the requirements of your specific procedure and in consideration of your preferences and your doctor’s best judgment.
What happens during breast reconstruction surgery?
Step 1 – Anesthesia
Medications are administered for your comfort during the surgical procedure. The choices include intravenous sedation and general anesthesia. Your doctor will recommend the best choice for you.
Step 2 – Flap techniques reposition a woman’s own muscle, fat and skin to create or cover the breast mound.
Sometimes a mastectomy or radiation therapy will leave insufficient tissue on the chest wall to cover and support a breast implant. The use of a breast implant for reconstruction almost always requires either a flap technique or tissue expansion.
A TRAM flap uses donor muscle, fat and skin from a woman’s abdomen to reconstruct the breast. The flap may either remain attached to the original blood supply and be tunneled up through the chest wall, or be completely detached, and formed into a breast mound.
Alternatively, your surgeon may choose the DIEP or SGAP flap techniques which do not use muscle but transport tissue to the chest from the abdomen or buttock.
.jpg)
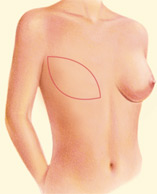
A latissimus dorsi flap uses muscle, fat and skin from the back tunneled to the mastectomy site and remains attached to its donor site, leaving blood supply intact.


Occasionally, the flap can reconstruct a complete breast mound, but often provides the muscle and tissue necessary to cover and support a breast implant.

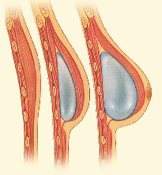
Step 3 – Tissue expansion stretches healthy skin to provide coverage for a breast implant.
Reconstruction with tissue expansion allows an easier recovery than flap procedures, but it is a more lengthy reconstruction process.
It requires many office visits over 4-6 months after placement of the expander to slowly fill the device through an internal valve to expand the skin.
A second surgical procedure will be needed to replace the expander if it is not designed to serve as a permanent implant.
Step 4 – Surgical placement of a breast implant creates a breast mound.
A breast implant can be an addition or alternative to flap techniques. Saline and silicone implants are available for reconstruction.
Your surgeon will help you decide what is best for you. Reconstruction with an implant alone usually requires tissue expansion.
Step 5 – Grafting and other specialized techniques create a nipple and areola.
Breast reconstruction is completed through a variety of techniques that reconstruct the nipple and areola.
 Following your surgery for flap techniques and/or the insertion of an implant, gauze or bandages will be applied to your incisions.
Following your surgery for flap techniques and/or the insertion of an implant, gauze or bandages will be applied to your incisions.
An elastic bandage or support bra will minimize swelling and support the reconstructed breast. A small, thin tube may be temporarily placed under the skin to drain any excess blood or fluid.
A pain pump may also be used to reduce the need for narcotics.
You will be given specific instructions that may include: How to care for your surgical site(s) following surgery, medications to apply or take orally to aid healing and reduce the risk of infection, specific concerns to look for at the surgical site or in your general health, and when to follow up with your plastic surgeon.
Be sure to ask your plastic surgeon specific questions about what you can expect during your individual recovery period.
- Where will I be taken after my surgery is complete?
- What medication will I be given or prescribed after surgery?
- Will I have dressings/bandages after surgery?
- When will they be removed?
- Will there be drains? For how long?
- When can I bathe or shower?
- When can I resume normal activity and exercise?
- When do I return for follow-up care?
Healing will continue for several weeks as swelling decreases and breast shape and position improve. Continue to follow your plastic surgeon’s instructions and attend follow-up visits as scheduled.
Results and outlook
The final results of breast reconstruction following mastectomy can help lessen the physical and emotional impact of mastectomy.
Over time, some breast sensation may return, and scar lines will improve, although they’ll never disappear completely.
There are trade-offs, but most women feel these are small compared to the large improvement in their quality of life and the ability to look and feel whole.
Careful monitoring of breast health through self-exam, mammography and other diagnostic techniques is essential to your long-term health.
When you go home
If you experience shortness of breath, chest pains, or unusual heart beats, seek medical attention immediately. Should any of these complications occur, you may require hospitalization and additional treatment.
The practice of medicine and surgery is not an exact science. Although good results are expected, there is no guarantee. In some situations, it may not be possible to achieve optimal results with a single surgical procedure and another surgery may be necessary.
Be careful
Following your physician’s instructions is key to the success of your surgery. It is important that the surgical incisions are not subjected to excessive force, abrasion, or motion during the time of healing. Your doctor will give you specific instructions on how to care for yourself.
 Cost is always a consideration in surgery. Prices for breast reconstruction can vary widely. A surgeon’s cost for breast reconstruction may vary based on his or her experience as well as geographic location.
Cost is always a consideration in surgery. Prices for breast reconstruction can vary widely. A surgeon’s cost for breast reconstruction may vary based on his or her experience as well as geographic location.
Many plastic surgeons offer patient financing plans, so be sure to ask.
Cost may include:
- Surgeon’s fee
- Hospital or surgical facility costs
- Anesthesia fees
- Prescriptions for medication
- Post-surgery garments, and
- Medical tests and x-rays
Breast reconstruction surgery after breast cancer is considered a reconstructive procedure and should be covered by health insurance. However, your coverage may only provide a small part of the total fee.
Your satisfaction involves more than a fee
When choosing a plastic surgeon for breast reconstruction, remember that the surgeon’s experience and your comfort with him or her are just as important as the final cost of the surgery.
- Areola: Pigmented skin surrounding the nipple.
- Breast augmentation: Also known as augmentation mammaplasty; breast enlargement by surgery.
- Breast lift: Also known as mastopexy; surgery to lift the breasts.
- Breast reduction: Reduction of breast size and breast lift by surgery.
- Capsular contracture: A complication of breast implant surgery which occurs when scar tissue that normally forms around the implant tightens and squeezes the implant and becomes firm.
- DIEP flap: Deep Inferior Epigastric perforator flap which takes tissue from the abdomen.
- Donor site: An area of your body where the surgeon harvests skin, muscle and fat to reconstruct your breast – commonly located in less exposed areas of the body such as the back, abdomen or buttocks.
- Flap techniques: Surgical techniques used to reposition your own skin, muscle and fat to reconstruct or cover your breast.
- General anesthesia: Drugs and/or gases used during an operation to relieve pain and alter consciousness.
- Grafting: A surgical technique to recreate your nipple and areola.
- Hematoma: Blood pooling beneath the skin.
- Intravenous sedation: Sedatives administered by injection into a vein to help you relax.
- Latissimus dorsi flap technique: A surgical technique that uses muscle, fat and skin tunneled under the skin and tissue of a woman’s back to the reconstructed breast and remains attached to its donor site, leaving blood supply intact.
- Local anesthesia: A drug injected directly to the site of an incision during an operation to relieve pain.
- Mastectomy: The removal of the whole breast, typically to rid the body of cancer.
- SGAP flap: Superior Gluteal Artery perforator flap which takes tissue from the buttock.
- Tissue expansion: A surgical technique to stretch your own healthy tissue and create new skin to provide coverage for a breast implant.
- TRAM flap: Also known as transverse rectus abdominus musculocutaneous flap, a surgical technique that uses muscle, fat and skin from your own abdomen to reconstruct the breast.
- Transaxillary incision: An incision made in the underarm area.
Use this checklist as a guide during your consultation
- Are you certified by the American Board of Plastic Surgery?
- Were you trained specifically in the field of plastic surgery?
- How many years of plastic surgery training have you had?
- Do you have hospital privileges to perform this procedure?
- If so, at which hospitals?
- Is the office-based surgical facility accredited by a nationally- or state-recognized accrediting agency, or is it state-licensed or Medicare-certified?
- Am I a good candidate for this procedure?
- What will be expected of me to get the best results?
- Where and how will you perform my procedure?
- What surgical technique is recommended for me?
- How long of a recovery period can I expect, and what kind of help will I need during my recovery?
- What are the risks and complications associated with my procedure?
- How are complications handled?
- What are my options if I am dissatisfied with the outcome?
- Do you have before-and-after photos I can look at for this procedure and what results are reasonable for me?
Plastic surgery involves many choices. The first and most important is selecting a surgeon you can trust.
Choosing an ASPS Member Surgeon ensures that you have selected a physician who:
- Has completed at least five years of surgical training with a minimum of two years in plastic surgery.
- Is trained and experienced in all plastic surgery procedures, including breast, body, face and reconstruction.
- Operates only in accredited medical facilities
- Adheres to a strict code of ethics.
- Fulfills continuing medical education requirements, including standards and innovations in patient safety.
- Is board certified by The American Board of Plastic Surgery or in Canada by the Royal College of Physicians and Surgeons of Canada®.
ASPS Member Surgeons are your partners in cosmetic and reconstructive plastic surgery.
Look for the ASPS Member Surgeon logo.

 The American Society of Plastic Surgeons and the Plastic Surgery Educational Foundation support National Breast Cancer Awareness Month each October.
The American Society of Plastic Surgeons and the Plastic Surgery Educational Foundation support National Breast Cancer Awareness Month each October.
ASPS has put together the following resources for people with breast cancer, including treatment options and legislative initiatives. The resources on this page include links to letters from patients who have had breast reconstruction following mastectomy, a variety of ASPS/PSEF publications about breast cancer and breast reconstruction and a list of links to other online breast cancer support organizations.
According to the American Cancer Society, more than 210,000 women in the United States were diagnosed with invasive breast cancer in 2005, and over 40,000 will die from the disease. Fortunately, improvements in post-surgical therapies are helping give more women the courage to get tested and get treated.
ASPS is working to increase awareness of breast reconstruction options available to breast cancer patients, and reminds women to schedule regular cancer screenings.
 3510 N. Ridge Rd, Suite 100
3510 N. Ridge Rd, Suite 100